The U.S. Department of Defense (DOD) is taking steps to explore how noninvasive, nondrug light therapy can help military members and veterans recover from traumatic brain injuries (TBI).
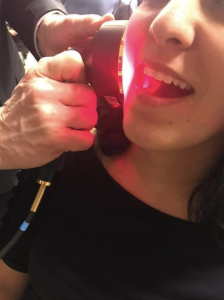
Transcranial photobiomodulation (PBM) uses red- and near-infrared light rays to stimulate mitochondria to restore cell function. The technology is rapidly showing promise in treating a variety of medical conditions such as drug addiction, pain, and mental health disorders.
Possible Clinical Trial
At the invitation of the DOD’s Congressionally Directed Medical Research Program, Paulo Cassano, M.D., Ph.D. and his PBM team in the Neuropsychiatry and Neuromodulation Division at Massachusetts General Hospital in Boston are applying for a grant to perform a randomized, double-blind, sham-controlled clinical trial on 96 subjects who have suffered from TBI effects for at least one year.

(Photo courtesy, Massachusetts General Hospital)
The study will look at how office and at-home PBM treatments can improve executive function and memory and control anxiety and sleep disturbances commonly experienced by individuals who received violent or repeated blows to the head or suffered from weapon reverberation during combat and training.
A bipartisan panel of U.S. House and Senate legislators has been pushing the military to do more to treat TBI.
Accelerating Interest
PBM emerged as a possible treatment modality in 1967, but only in the last 15 years have researchers been studying it as a therapy for brain injuries. Studies on mice have shown PBM can restore motor function. There is anecdotal evidence it can be effective on humans.
“In Canada, children injured to the point of disorientation showed spectacular recovery in less than one week after being treated with PBM,” Cassano told Health Care News. “So, there is growing evidence that it works. The missing piece is showing whether there is a clinical benefit in a sufficient sample size.”
PBM has been used on more than 100 million patients without documented side effects, the PBM Foundation states. There have been more than 1,000 randomized clinical trials and 9,000 research studies on PBM, many published in leading medical journals and registered with the National Institutes of Health.
Portable, Immediate Treatment
The Journal of the American Medical Association lists PBM as one of the first options for treating pain. The VA recommends PBM for treating neurological conditions in vets. The DOD uses PBM in its warfighter effectiveness program.
Leading cancer centers use PBM to treat pain, and there is an ongoing study to see if PBM can reduce cravings and depression from opioid addiction.
“Mass General has over 600 professionals interested in PBM,” said Cassano. “We aspire to have neurostimulation play a role at the scene in an ambulance or the periphery of the football field so that treatment can be beneficial right away.
“We know some lesions are related to the immediate hit, but some injury is related to the brain’s response to the hit, the inflammation, and we want to prevent those secondary lesions,” said Cassano.
‘Scalable’ Mental Health Care
The low cost, ease of use, and portability of PBM can help with the growing shortage of psychiatrists and greater demand for mental health.
“We want interventions that are scalable, that could potentially be applied to a location, the warzone for example, and scalable in terms of number of people that can be treated,” said Cassano.
Cassano plans to study whether patients can get the same results from a wearable device as office devices, which are generally heavier and bulkier and require a technician.
“If the office device is a winner, we can work and understand what it takes to deploy those devices,” said Cassano.
‘Future of Psychiatry’
The mainstay of mental health treatment today is medication, which can cause major side effects, and psychotherapy, which is labor-intensive and takes a long time.
“Psychotherapy can be very effective, but it is difficult to scale,” said Cassano. “It is difficult to find providers who have the level of training on evidence-based psychotherapy, to deal with things like [post-traumatic stress disorder], depression, or emotional dysregulation, and even if they have that care, they still may not achieve total recovery.”
Like PBM, electroconvulsive therapy and transcranial magnetic stimulation work on the cellular level. Those treatments involve anesthesia.
“We know that neurostimulation is tremendously effective for many conditions, including depression,” said Cassano. “We need to find a way to bring this treatment outside the office, and the data is showing these treatments are effective.
“You want to accumulate sufficient data if you’re going to scale it to the public,” said Cassano. “This is the future of psychiatry. Psychiatrists will be trained to prescribe this treatment, and because these treatments are safe and have nonsignificant risk” according to the U.S. Food and Drug Administration (FDA), “some of these low-dose devices will be available for wellness, as they are already.”
Regulatory Hurdles
Although the FDA has approved PBM for a variety of medical conditions, there is still room for wider application, says Scot Faulkner, an advisor to the PBM Foundation.
(Photo, courtesy of the PBM Foundation)
“The FDA still talks about photobiomodulation as a non-heating heating lamp,” said Faulkner. “In terms of formal indication for use, it is still only there for general wellness, not specific indications. It is not being fully reimbursed [by insurers]. We are hoping to work through that with Medicare and perhaps a national coverage determination.”
It is also important to develop a certification process for devices, many of which are sold by the thousands on the internet, says Faulkner.
“Studies have shown consistency is all over the map,” said Faulkner. “Many devices coming out of China have no quality control. It does everyone a disservice, because if someone is presenting it as red-light therapy and it doesn’t work, then they are going to be a skeptic and believe PBM doesn’t work.”
AnneMarie Schieber ([email protected]) is the managing editor of Health Care News.
For related article, click here.



