Florida lawmakers are considering a bill that would empower health care providers to prescribe the best-suited medications for Floridians on Medicaid suffering from “serious mental illnesses” without having to initially prescribe possibly inferior, cheaper medications.
The bill, SB 264, “would create an exception to what is known as ‘step therapy’ for a series of psychiatric conditions, such as bipolar disorders, major depressive disorders and obsessive compulsive disorders,” Florida Health News reports.
Under current law, Florida doctors must follow what is called “step therapy,” which mandates that Florida’s “Medicaid program uses a ‘preferred drug list,’ with drugs on the list also tied to rebates offered by drug manufacturers.”
“If doctors determine it is necessary to prescribe drugs not on the preferred list, it triggers prior-authorization and step therapy requirements. Generally, that means trying less-expensive drugs before moving to drugs that cost more.”
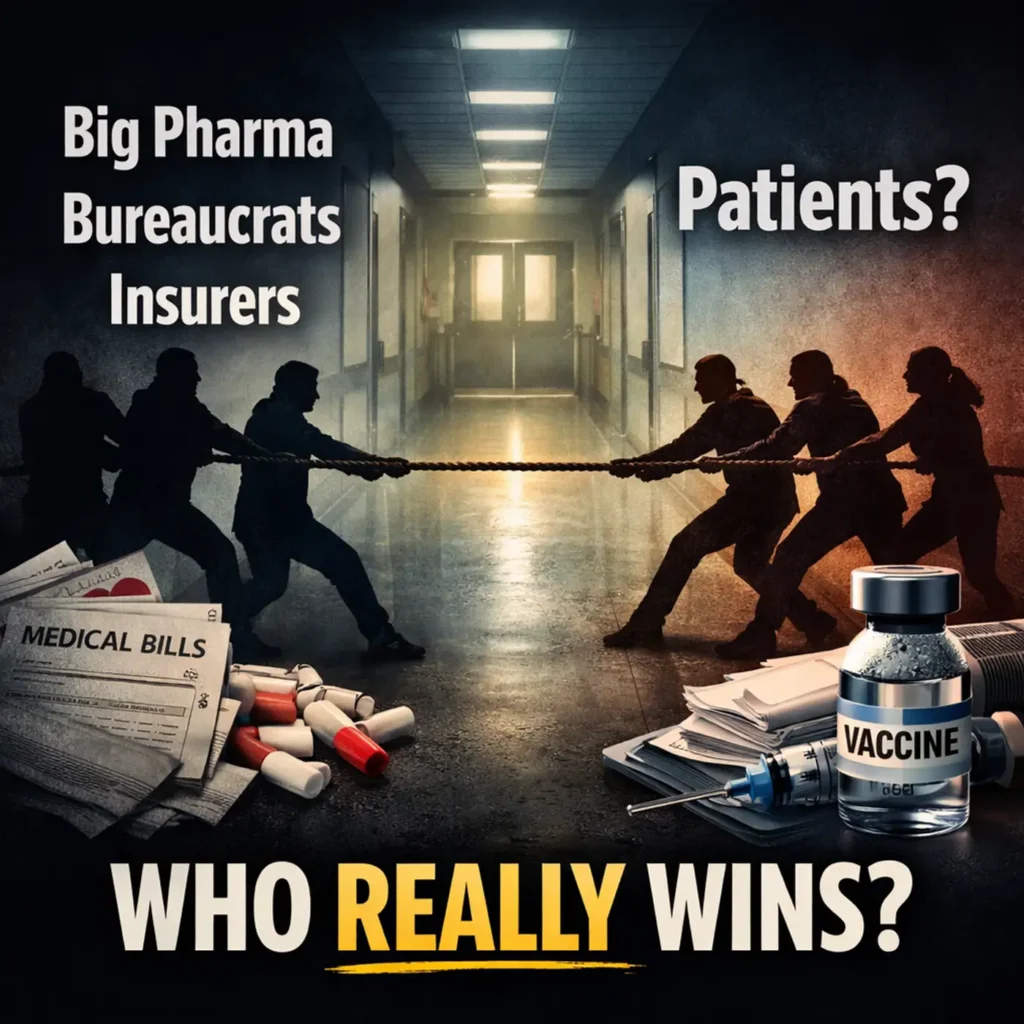
Also known as “fail first,” step therapy is a policy developed by health insurers that is intended to control costs” by limiting the medications doctors can prescribe as a first course of treatment.
Opponents of step therapy contend that the policy does not save money, puts peoples’ health in jeopardy, and “generates miles of red tape.” Moreover, they argue that it grants too much power to health insurers and other third-party payers, who almost always try to drive down costs rather than putting the patients’ best interests first.
According to a 2021 study published in Health Economics, Policy and Law, “step therapy was designed as a cost savings measure to prevent overuse of expensive treatments in favor of more cost-effective options. The above example of IBD treatments suggest this may be short-sighted, saving immediate costs only to incur complications with potentially increased long-term costs of less effective medications.”
“There is other evidence from multiple areas of medicine that step-therapy policies shift, rather than reduce, costs,” the study notes. “A study on the use of step-therapy protocols for antihypertensive medications showed there was an initial decrease in the amount spent on medication that was offset by an approximate increase of $400/year in costs paid directly by patients.”
The legislation, which is under consideration in the Florida House and Senate (SB 264), would require “the Agency for Health Care Administration to approve drug products for Medicaid recipients for the treatment of serious mental illness without step-therapy prior authorization under certain circumstances.”
Serious mental illness, according to the bill, is defined as “any of the following psychiatric disorders as defined by the American Psychiatric Association in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition: (a) Bipolar disorders, including hypomanic, manic, depressive, and mixed-feature episodes. (b) Depression in childhood or adolescence. (c) Major depressive disorders, including single and recurrent depressive episodes. (d) Obsessive-compulsive disorders. (e) Paranoid personality disorder or other psychotic disorders. (f) Schizoaffective disorders, including bipolar or depressive symptoms. [and] (g) Schizophrenia.”
The overall goal of the bill is simple: ensure the “delivery of quality medical care” in a cost-effective manner.
Step therapy is very similar to prior authorization (PA), which “has become increasingly common as insurance companies try to keep a lid on skyrocketing drug costs.” However, as explained in The Heartland Institute’s American Health Care Plan: State Solutions, “PA requires that doctors receive permission from an insurance company before prescribing (typically more expensive) medication that may be the choice of the doctor and best for the patient.”
“Patients are often put through a trial of inferior or even unhelpful drugs while precious time ticks away. This forces doctors and staff to take valuable time to lobby for the appropriate medication through the convoluted prior authorization process.”
Nine states and the District of Columbia have passed PA reform legislation in recent years. By doing so, these states, which includes deep-blue Massachusetts, are putting patients first by eliminating the arduous process to receive the proper medication that is best-suited to treat their condition. By dismissing or reforming PA and step therapy, patients no longer need to “earn” the right to obtain the medication or care that they need.
The following documents provide additional information about step therapy and prior authorization reform:
An act relating to step-therapy protocols requiring the Agency for Health Care Administration to approve drug products for Medicaid recipients for the treatment of serious mental illness without step-therapy prior authorization under certain circumstances.
Florida bill would create Medicaid exception to ‘step therapy’ for psychiatric medications
A state Senate committee advanced a measure that would allow doctors to prescribe appropriate meds to patients with mental illnesses without having to first use other drugs that are not effective.
American Health Care Plan: State Solutions
Researchers from The Heartland Institute explain what states can do to make health care more accessible and affordable while awaiting a comprehensive federal plan to replace the current outdated, wasteful, access-denying, government-warped health care system.
Do patients benefit from legislation regulating step therapy?
Step therapy, also termed fail-first policy, describes a practice of insurance and pharmacy benefit management companies denying reimbursement for a specific treatment until after other treatments have first been found ineffective (i.e. failed).