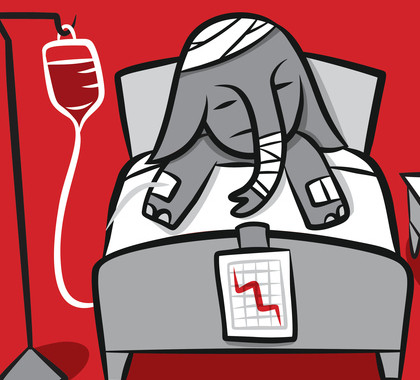
The House of Representatives is poised to decide the fate of the American Health Care Act (AHCA), the Obamacare replacement plan backed by House GOP leadership and President Donald Trump. Speaker Paul Ryan (R-WI) has called the moment a “rendezvous with destiny.” Trump has said Republicans could lose seats in 2018 if they reject the bill. And conservative Republicans think they’ll lose seats if they pass the bill.
“I think if we do vote for this we will lose the majority,” Rep. Mo Brooks (R-AL) told Bloomberg Politics after a closed-door meeting between Trump and House Republicans on March 20. Brooks is a member of the House Freedom Caucus, whose members could stop AHCA from obtaining the 218 votes needed to pass the chamber. The bill will fail if 21 Republicans join House Democrats to reject it.
If AHCA does end up on Trump’s desk, Republicans can guarantee Democrat wins in 2018 and 2020 by continuing to fail to change the American people’s understanding of what health insurance is for.
Congress and most patients assume it is financially prudent to submit health insurance claims every time one receives medical care. The same assumption drives health care costs and insurance premiums higher each year and renders every health care reform bill passed by Democrats and Republicans in Washington, DC a health insurance reform bill.
Republican reformers have a challenge before them Democrats didn’t. Obamacare capitalized on the conventional wisdom, which says the sensible and financially sound way to pay for health care is first to pay health insurance premiums. Second, if you do get sick or injured, file an insurance claim by handing your provider your insurance card the moment you walk in the door. Third, pay an obscenely high price for care. Fourth, exhale relief: You are that much closer to meeting your annual deductible, after which you’ll enjoy the illusion of free health care, if you get sick or injured again between now and January 1.
The Affordable Care Act is the shrine to this mentality, where Democrats and Republicans alike splice hands in the unholy worship of health insurance. Obamacare’s individual mandate and tax penalty served as temple guards, coercing people to buy insurance covering almost every condition under the sun.
Now Republicans hover on the precipice of legalizing the sale of inexpensive, or at least less expensive, health insurance. Technically, no one would have to buy it. Out with Obamacare’s temple guard, in with the GOP’s rent-a-cop: The GOP would replace the individual mandate and tax penalty with a 30 percent insurance premium surcharge for people buying insurance after experiencing a lapse in coverage.
But insurance is still god under AHCA. Insurance is so important, the Republican plan would give a mostly age-based tax credit worth $2,000 to $4,000 per buyer, and up to $14,000 per family, for individuals with an adjusted gross income (AGI) of up to $75,000 and married couples with an AGI of up to $150,000. Smaller credits await households with greater incomes.
Even if the GOP plan is politically expedient following seven years of Obamacare entitlement brainwashing, Republicans will have a bigger political challenge if AHCA passes. Many of the low-premium insurance plans Republican reformers want will probably have much higher deductibles than even an Obamacare bronze-level plan, roughly $6,000 per person or $13,000 per family.
To weather these high deductibles politically, Republicans must un-deify health insurance. They must refute the conventional wisdom that chasing a deductible every time a medical need arises is rational or frugal.
Republicans must persuade Americans to view health insurance as nothing more than insurance–a thing rarely used to pay for anything but catastrophes. Like an auto, homeowners, or life insurance policy, health insurance will become affordable when people stop filing claims except in the medical equivalent of car wrecks, house fires, or death of a spouse.
The more individuals view health insurance as mere insurance instead of a holy health care payment plan, the more individuals will shop for health care the way they shop for every other service. People will Google for nearby providers, call two or more, ask for the lowest possible price for someone not paying with insurance, and decide based on value which provider to see. Providers charge such self-pay patients 25 to 90 percent less than what they charge insured patients–a fact I personally verified by tallying my family’s 2016 medical bills the other night.
The brave new world Republican reformers should be, and may be, steering us toward is one where patients negotiate cheap health care prices with doctors, while paying cheap premiums and putting insurance out of their minds until catastrophe strikes. That’s a lot better than the Obamacare norm–having expensive insurance you’re always trying to use but which never benefits you, because you’re always paying the prices doctors charge insured patients and still never reach your deductible.
It’s just not enough for Republicans to sell AHCA, or any bill resulting in the sale of inexpensive insurance policies. To survive politically, Republicans must also persuade relatively healthy Americans health insurance is mere insurance, not a spiritual rite.
— Michael T. Hamilton ([email protected], @MikeFreeMarket) is a Heartland Institute research fellow and managing editor of Health Care News, author of the weekly Consumer Power Report, and host of the Health Care News Podcast.
IN THIS ISSUE:
HOW WOULD PROPOSED AMENDMENTS CHANGE THE REPUBLICAN HEALTH CARE BILL?
President Trump bragged that he won over many new converts to House Republicans’ “repeal-and-replace” legislation following a Friday meeting with Members of Congress at the White House. After the meeting, House leaders scheduled a vote for later this week on the measure, and introduced provisions implementing the agreement in a managers amendment package late last night.
So what tweaks did Trump promise to Congress members on Friday–and will they improve or detract from the legislation itself?
The agreement in principle with the House Members includes several components:
1. Abortion restrictions for Health Savings Accounts (HSAs): RSC Chairman Mark Walker (R-NC) and other pro-life members asked for further restrictions on abortion funding. As a result, the agreement eliminates language allowing unspent tax credit dollars to get transferred into health savings accounts, for fear those taxpayer dollars moved into HSAs could be used to cover abortions. However, as I noted recently, many of the other restrictions on taxpayer funding of abortion could well get stripped in the Senate, consistent with past precedent indicating that pro-life riders are incidental in their budgetary impact, and thus subject to the Senate’s “Byrd rule” preventing their inclusion on budget reconciliation.
2. Prohibiting more states from expanding Medicaid: While this provision has been sold as ensuring no new states would expand Medicaid to able-bodied people, it does not do so–it only ensures that states that decide to expand after March 1 will receive the regular federal match levels for their able-bodied populations (i.e., not the 90-95 percent enhanced match). Neither the bill nor the managers package permanently ends the expansion to able-bodied adults–which the 2015/2016 reconciliation bill did–or ends the enhanced federal match for expansion states until January 2020, nearly three years from now.
3. Medicaid work requirements: The agreement permits–but does not require–states to impose work requirements, a point of contention between some states and the Obama Administration. However, non-expansion states will have comparatively few beneficiaries on which to impose such requirements. Medicaid programs in non-expansion states consist largely of pregnant women, children, and elderly or disabled beneficiaries, very few of whom would qualify for the work requirements in the first place.
The fourth component–allowing states to take their federal payments from a reformed Medicaid program as a block grant, instead of a per capita cap–warrants greater examination. In general, per capita caps have been viewed as a compromise between the current Medicaid program and a straight block grant fixed allotment. In the 1994-95 budget showdown with then-House Speaker Newt Gingrich, President Clinton proposed per capita caps for Medicaid as an alternative to the Republican House’s block grant plan. …
If Medicaid reforms comprised the entirety of the bill, they would likely be worth supporting, despite the complexities associated with the debate between expansion and non-expansion states. The move to per capita caps represents significant entitlement reform, and is consistent with the principles of federalism. …
As a repeal bill, however, the measure as currently constituted falls short. The agreement on Friday made zero progress on repealing any other insurance benefit mandates in Obamacare–the primary drivers of higher premiums under the law. That’s one reason why CBO believes premiums will actually rise by 15-20 percent over the next two years. House leadership claims that the mandates must remain in place due to the procedural strictures of budget reconciliation in the Senate. But the inconsistencies in their bill–which repeals one of the mandates, modifies others, and leaves most others fully intact–contradict that rhetoric.
Moreover, by modifying rather than repealing some of the Obamacare mandates, the bill preserves the Washington-centered regulatory structure created by the law, undermining federalism and Tenth Amendment principles. …
SOURCE: Chris Jacobs, The Federalist
MICHIGAN MEDICAID PATIENT CAN’T FIND CARE, SO SHE PAYS FOR INNOVATIVE ALTERNATIVE
When Michigan expanded Medicaid in 2013, one person who was relieved was cancer survivor and self-employed child care provider, Dani Valassis.
“I wasn’t making enough money to afford good, quality care,” said Valassis, who was seeking new health insurance after a divorce. When she learned she qualified for “Healthy Michigan,” this state’s version of the Medicaid expansion component of the Affordable Care Act, she thought her coverage woes were over until she sought routine care. …
“It was just frustrating. I felt like I was cattle,” said Valassis. …
She thought there was no way she could afford the visits until she learned her physician, Dr. Chad Savage, was using a new billing model known as direct primary care.
“You pay a flat fee. You can see him as often as you want, and we can communicate on the internet and it’s amazing,” said Valassis.
Valassis pays $49 a month. Younger patients pay even less. Savage can offer care for that price because he no longer spends time and money processing insurance claims.
He added that when he left the insurance-based system, his costs dropped by more than half. …
Because of its promise to both doctors and patients, direct primary care has captured the attention of lawmakers, not just for Medicaid, which costs taxpayers billions, but for government workers.
“If we can find a way to go off and provide better care for less money, that’s where you start,” said Sen. Patrick Colbeck, R-Canton.
Colbeck wants Michigan to conduct a pilot program using direct primary care with a small group of Medicaid patients. He believes not only could it be instructive for state government but for anyone who pays for health insurance. Michigan’s private sector spends over $35 million a year on health care, according to the Kaiser Family Foundation. Initial studies of direct primary care show that it can reduce health care costs by at least 18 percent. …
SOURCE: Anne Schieber Dykstra, Michigan Capitol Confidential
OHIO PROGRAM EXPANDS HEALTH AND DENTAL CARE ACCESS FOR RURAL PATIENTS
Dr. Darcy Cook is the face of a health-care transformation taking hold in medically underserved Perry County.
Cook could have practiced anywhere after she graduated last year from Ohio State University’s College of Dentistry. But the daughter of Appalachian Ohio was intent on returning to her home region to practice. She is needed.
Cook works at the Hopewell Health Center in McArthur in Vinton County. She plans to move to the Hopewell Health Center in New Lexington in Perry County when that clinic opens a dental wing this year. It also will provide clinical training to students studying to become dental hygienists in a new program that Hocking College plans to start next year.
The emerging, interwoven plans all are part of a strong push to increase access to health care in Perry County, while also educating and training the local workforce for jobs in the health field. …
Appalachian Ohio children have a nearly 60 percent higher rate of tooth decay than Ohio as a whole. There also are fewer dentists. There is one dentist per 1,874 people in Ohio. But in the Appalachian part of the state, the numbers are one per 3,138 people, Smith said.
“We need to help with education,” she said. “It’s not just access to care. We need to do a better job getting oral-health education out there. Some people are under the impression that you only see a dentist when you have a toothache, instead of going twice a year to prevent that toothache.”
Cook is looking forward to helping train the 20 students expected to initially enroll in the Hocking College program. Dental hygienists clean teeth, help with imaging and provide patient education. …
SOURCE: Mary Beth Lane, The Columbus Dispatch
NORTH CAROLINA LAWMAKERS EYE TELEMEDICINE PAYMENT PARITY
Lawmakers in North Carolina – a state with a long track record of telemedicine and mHealth innovation – are poised to debate a bill that would establish reimbursement parity for payers.
H.B. 283 would mandate that health plans cover telemedicine services as they would in-person treatment, and would prohibit insurers from denying the service simply because it isn’t provided in-person. In addition, insurers wouldn’t be able to limit where the service is provided.
The bill’s primary sponsor, Republican Congressman Donny Lambeth of Forsyth, said the bill addresses a lack of healthcare access for residents in rural areas of the state. He told the Winston-Salem Journal the state suffers from a “two-tiered system of care,” with remote areas “struggling” to provide adequate healthcare.
“With the sophistication of technology, you can link many rural locations into some of the world’s best healthcare,” he said. “If the large systems invest in this new technology and link back into the less populated areas and can get paid for those services, then I believe we have made a significant improvement in caring for persons in rural areas who currently go untreated.”
According to the American Telemedicine Association, 31 states and the District of Columbia mandate reimbursement parity for telemedicine, and at least five states are debating the concept. Other states aren’t as receptive, with payers leading the argument that they should be the ones to set payment rates for an industry still trying to figure its value.
“Clearly, the costs are lower when it’s telemedicine, so the reimbursements should be lower,” said Jon Hurst, president of the Retailers Association of Massachusetts, who helped repel that state’s bid for a parity law last year.
“It’s mostly a vehicle for making sure that people who want to do telemedicine on whatever terms they make up and charge what they want will get away with it,” added Jim Kessler, general counsel for Health New England, based in Springfield. “If you mandate certain services and reimbursements, you’re taking away the whole negotiating ability of health insurers to benefit consumers.”
Earlier this year Nebraska lawmakers submitted a bill for telemedicine parity, making the same argument as their colleagues in North Carolina.
SOURCE: mHealthIntelligence.com.