Consumer Power Report #325
In keeping with the Obama administration’s solutions when it comes to policy problems in other areas, its latest response to the challenge of health care costs is simple: Spend more money. The latest example comes in the form of a major bet by the White House on Oregon’s proposed Medicaid alterations, approved last week in a surprising decision. The cost to taxpayers? $1.9 billion:
It all, however, does hinge on a very big “if”: No other state has ever tried what Oregon is about to try. It is, however, an approach many health care payers are thinking about: It’s how Massachusetts wants to bring down health costs in private insurance, and the federal government’s plan [to] rein in Medicare spending. Oregon could, in many ways, serve as a test case for other cost control efforts.
Oregon wants to move its 600,000 Medicaid populations into “Coordinated Care Organizations.” These are health care systems that will accept a flat fee for all care delivered. While remaining within that budget, they will have to hit certain quality metrics, ideally creating financial incentives to deliver the most cost-effective care that can deliver good results.
If this idea sounds familiar, that’s because it shows up in the Affordable Care Act: Accountable Care Organizations will use a similar structure within the Medicare program (albeit with some differences in oversight and governance).
If the Coordinated Care Organizations, or CCOs, can hit the metrics and stay within the budget, they will net the savings. If care costs more than the flat fee, the health care system will be on the hook for additional spending.
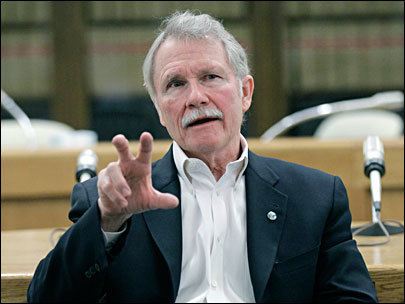
But as always, this could be an example of a temporary fix–you might even call it a bailout–which turns into a long-term boondoggle, a fact Democratic Gov. John Kitzhaber acknowledged.
“The only thing that stands between this state and success is ourselves,” [Gov. Kitzhaber] said, standing in a third-floor meeting room of the nonprofit care group, Central City Concern.
The public event amounted to a victory lap after Kitzhaber returned from Washington D.C. with agreement for the federal funds. Earlier in the week he’d scrapped all meetings to fly east amid rumors that funding previously characterized as a done deal might suddenly disappear. The federal money amounts to a down payment on savings Oregon intends to deliver the federal government of $11 billion over the rest of the decade.
The five-year deal provides a large chunk of funds this year: $620 million. That nearly covers a $640 million budget hole that was built in to the state’s current budget by lawmakers using theoretical savings to comply with the constitutional requirement of passing a balanced budget.
The truth is that this approach to cost controls has never been proven to work, and it is likely to have unanticipated and negative consequences for the quality of care. But Oregon also could prove to be a test case for post-Obamacare reforms should the president’s law withstand the legal review at the Supreme Court. Should Oregon succeed, or even deliver a portion of the savings it has promised, it may very well be that future Americans will find themselves in these CCOs–powerless to operate within anything more than what is essentially a public utility disguised as a health care provider.
— Benjamin Domenech
IN THIS ISSUE:
MASSACHUSETTS SENATE TO UNVEIL GLOBAL PAYMENT BILL
The inability of Mitt Romney’s 2006 reforms to reduce health care costs comes due, in the form of a shift to global payments almost assured of passage given the monopartisan nature of the Massachusetts legislature.
The Massachusetts Senate is preparing to release a health care financing bill just days after House leaders unveiled their version of the bill.
House leaders said Friday that their bill will lower family premiums by nearly $2,000 annually over the next five years by cutting waste and inefficiency out of the health care system.
The House bill is also designed to reward doctors and hospitals for keeping patients healthy instead of paying them for each operation or service they provide.
The Senate is expected to unveil its version of the bill this week and vote on it the following week.
Senate President Therese Murray has said she expects passage by July 1.
Gov. Deval Patrick first proposed in 2010 that the state move toward a so-called global payment system to replace the fee-for-service approach.
For more on the subject, read this from the Wall Street Journal.
The Massachusetts House proposal would peg overall state health spending growth at the gross state product’s annual rate of increase through 2015. Starting in 2016, the target rate would drop to a half-percentage point below GSP’s yearly rise. That could represent a significant cutback: historically, health spending at both the state and the federal level has risen at a higher rate than gross domestic product.
The bill would include the health spending tied to every state resident, no matter how they get their health coverage, though it wouldn’t count money consumers spend on their own outside their main insurance.
In addition to monitoring the health-spending growth rate, the new health authority would come up with alternative models for how medical providers should be paid that avoid the fee-for-service style in which volume generates more reimbursement. Insurers’ contracts with providers would eventually be required to generally move away from fee-for-service. …
The bill includes a provision that would require providers that are getting more than 20% above the median price for a service to justify the rate or potentially pay a surcharge.
SOURCE: BostonHerald.com
ILLINOIS SUSPENDS OBAMACARE EXCHANGE
Illinois Democrats decide to wait and see what the Supreme Court says:
“I’ve suspended the talks on the Illinois insurance exchange until the Supreme Court makes its decision, which we expect in June,” Rep. Frank Mautino (D- Spring Valley), who has been leading Illinois’ talks to set up the exchange, said.
“As the negotiator, it’s very difficult to have … businesses – decide how much they’re willing to pay to run an exchange, when the federal law may go away. So I’ve lost a lot of the strength of negotiation,” he said.
Controversial aspects include who’ll run the exchange, how much power insurance companies will get, and who’ll pay for it. About 50 organizations, including insurance companies, business groups, and health care advocates had been meeting weekly.
SOURCE: Cato Institute
COULD MEDICAID REALLY COLLAPSE THE ILLINOIS BUDGET?
The AP investigates and finds: Yes, it could.
Q: Could Medicaid really “collapse” if the system isn’t reformed, as Quinn claims?
A: Yes, according to Laurence Msall, president of the nonpartisan Civic Federation. That would mean doctors refusing to accept Medicaid patients, safety net hospitals closing because of unpaid bills and poor people going without health care, he said. Social service providers that serve the elderly and developmentally disabled could close their doors.
In addition, the state could face further downgrades in its credit ratings, making it difficult or impossible for the government to borrow money.
“It would be a financial disaster for anyone who does business with or interacts with the state of Illinois, not just for our most vulnerable, but also for school districts, local governments and participants in other state programs,” Msall said.
Illinois has used “accounting gimmickry” to delay paying for Medicaid services, perhaps more than any other state, he said. Perhaps no other state has allowed its unpaid bills to pile as high. The pile could possibly grow $21 billion by 2017 unless the state takes action.
SOURCE: Quad-City Times
NEW HAMPSHIRE SENATE VOTES ON STUDYING COMPACT OPTION
New Hampshire is about to become the most recent state to vote on the Health Care Compact concept, a structure that may be the next legal confrontation with Obamacare should the Supreme Court rule in its favor.
The Senate is considering whether New Hampshire should form an interstate compact to assume control for health care within state boundaries.
The House passed the bill in March that proposes that New Hampshire join with other states in delivering health care to its residents. Under the bill, the states would receive block grants from the federal government and would take over Medicare and Medicaid. Congress would have to approve the compact for it to take effect.
House Republican Leader D.J. Bettencourt sponsored the bill which seeks to free the state from the mandates of the Patient Protection and Affordable Care Act. The bill would supersede any federal health care law.
The Senate Health and Human Services Committee is recommending the Senate vote Wednesday to study the idea.
SOURCE: Fosters.com
KANSAS CONSIDERS PROTECTIONS FOR PHARMACISTS
The Kansas legislature considers protections for pharmacists in light of the recent conscience overruns from Washington.
In Lawrence, Kansas University’s Watkins Memorial Health Center allows pharmacists to refuse service for contraception but has a policy that “staff would seek out a willing employee” to fill the prescription, said Cathy Thrasher, pharmacist in charge at Watkins. Watkins would continue that policy if a bill under consideration in the state Legislature passes.
Similarly, Kmart, Walgreens, Walmart and CVS have corporate policies that essentially say pharmacists may refuse to fill a prescription, as long as he or she turns the customer over to another pharmacist in the building or refers the prescription to a nearby pharmacist. That’s the position the American Pharmacists Association, which governs ethics for the profession, has recommended since 2009.
But a bill under consideration in the Kansas House could allow pharmacists to refuse to fill prescriptions for contraception on moral grounds and would make Kansas one of nine states to legally protect a pharmacist’s right to refuse.
According to the bill, pharmacists who believe a drug may lead to an abortion could refuse service. The bill’s language gives the pharmacist too much leeway, say reproductive rights advocates, who argue the bill could result in drugs ranging from birth control to emergency contraception being refused.
SOURCE: LJWorld.com
GALEN INSTITUTE 2012 INNOVATIONS CONFERENCE
I encourage you to attend the Galen Institute’s event on Wednesday in Washington, D.C.
After a remarkable six hours of oral argument on ObamaCare before the Supreme Court, the stage is set for an historic ruling from the High Court on the future of the health law. The outcome will determine whether Washington continues to turn an infinite number of regulatory dials to try to control one sixth of our economy or whether innovation will be freed to allow transformative changes in medical technology, health care delivery, and financing.
We believe that freedom and the creative spirit will prevail.
Our fourth annual conference on the Value of Innovation in Health Care will showcase top experts from around the country and throughout the health sector who will tell us about the game-changing innovation to come. The Galen Institute never ceases in promoting policies that encourage innovation and patient-centered options for health care. Join us to learn about the exciting advances on the horizon.
Key policy leaders will be speaking at the session, which runs throughout the morning.
SOURCE: 4th Annual Conference on The Value of Innovation in Health Care
MARKUP: PRESCRIPTION DRUG USER FEE ACT
The House Energy and Commerce Committee will be marking up the PDUFA this week. A background memo covers the important points. For those wishing to attend:
The Subcommittee on Health markup originially scheduled for Thursday, April 26, 2012, has been rescheduled for Tuesday, May 8, 2012, at 10:00 a.m. in room 2123 of the Rayburn House Office Building to consider a Committee Print to reauthorize various FDA user fee programs.