Health insurance companies wanting to participate in the state exchanges mandated by President Obama’s health care law could have to compete under the table for political influence to gain access to the taxpayer-subsidized marketplace, as indicated by recent events in Missouri.
If a state selectively contracts participation in its exchange, artificially limiting the number of companies allowed in, there is potential for corruption, says Edmund Haislmaier, senior research fellow at The Heritage Foundation.
“The states, if they set up exchanges, have the flexibility to deal with this kind of thing, and so a state would be better off to have an ‘any willing insurer’ kind of approach, as opposed to a procurement kind of approach, where you’re trying to reduce the number of carriers,” Haislmaier said. “If you try to have selective contracting there is always the temptation for it to be political.”
Campaign Money Influences
Carl Bearden, executive director of citizen’s group United for Missouri, says an example of what could result took place recently in his state, which recently adopted managed care under its Medicaid program, in the process booting California-based Molina Healthcare from the system.
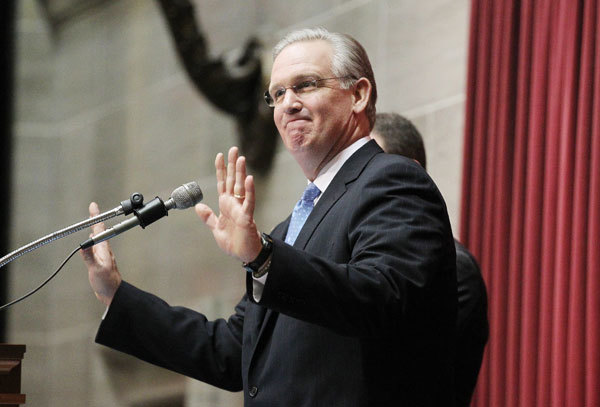
Molina’s Missouri division has sued, alleging state officials violated competitive bidding laws and changed the rules to favor another company, Centene Corp., which hasn’t been active in Missouri since 2006 but had recently donated $50,000 to the campaigns of Democratic Gov. Jay Nixon, $25,000 to Democratic Attorney General Chris Koster, $19,000 to Republican Auditor Tom Schweich, and thousands more to various legislative and statewide candidates.
Bearden says the Medicaid contract in question was for about $1.1 billion in services.
“They traditionally have awarded the contract for this particular delivery to any company that was willing to meet the going rate,” Bearden said. “One of the companies that’s been doing it for sixteen years didn’t get one, and one of the companies that did get one has been a recent campaign contributor to the governor.”
Bearden says such an approach exported to a health insurance exchange would raise costs and reduce availability.
“It’s tough to find providers in those rural areas, so when you open it up to companies charging the same rate, you would think that would be better for service providers in rural areas, but by limiting it you eliminate that service, ” Bearden said. “If the number of companies that can participate on the exchange is limited, then everybody’s worst nightmares come true, and you’re actually reducing availability of health care and driving up costs by restricting competition.”
Companies Vow to Participate
Steve O’Dell, senior vice president of Molina Healthcare, said his company will participate in the exchanges as long as they exist.
“Our position is pretty simple: We’re preparing for the health insurance exchanges because it is the law of the land at this point,” O’Dell said. “We will, if that changes, change our approach to it. But right now as a company we are going to participate in the exchanges.”
Molina says another complicating factor is the high number of people likely to move back and forth between Medicaid and the exchanges.
“The biggest problem that the states have, and the state agencies that we consider our biggest customers, is that they will have a tremendous amount of churn between Medicaid and the exchanges,” O’Dell said. “We’ve said that we will be on either end of the churn point. So we’ll participate in the health insurance exchanges.”
Public Opposes Exchanges
Patrick Ishmael, a policy analyst at the Missouri-based Show-Me Institute, says the issue may be moot.
“Issue one here still is whether Missouri implements an exchange,” Ishmael said, noting the state voted in a 2010 ballot initiative not to allow a health insurance mandate and the mood of voters is decidedly against participating in an exchange.
Haislmaier agrees, saying states with conservative political leadership are more likely to go with an any-willing-insurer approach, but they’re also more likely not to set up an exchange at all.
“To the extent that the state is dominated by liberals in the executive and legislature, they tend to prefer what’s called the selectively contracting approach,” Haislmaier said, noting corruption is “one of the potential abuses that could arise under a selective contracting approach, as abuse can arise under any selective contracting arrangement of any kind on any subject.
“We’re saying very strongly that you should use an any-willing-insurer approach,” Haislmaier advised.